Blog
Integrated Care: The Kaiser Healthcare Model
The Kaiser Permanente healthcare model first started in during WWII when Henry Kaiser created a healthcare program to serve his construction, mill, and shipyard employees. Less than a decade later, the program was open for public enrollment in 1945.
Fast forward 70 years and you'll find Kaiser is an award-winning institution that few companies have been able to replicate. They've recently announced $600,000 in grants for mental health and housing in Oregon and $22 million in grants to community organizations in three states—all of this while providing nationally recognized healthcare for their members.

It Starts with a Vision
Kaiser's "north star" is a very clear mission and vision embedded in their corporate culture:
Mission: To provide high-quality, affordable health-care services and improve the health of our members and the communities we serve.
Vision: We are trusted partners in total health, collaborating with people to help them thrive, creating communities that are among the healthiest in the nation, and inspiring greater health for America and the world.
These two guideposts have created a culture that unifies physicians, nurses, employees, and members. Kaiser's fast facts state that they have over 12 million members in eight markets, they recorded $79.7 billion in revenue for 2018. Kaiser has nearly 23,000 physicians and over 217,000 employees ready to serve their membership.
Successful Integrated Care
One of the reasons that Kaiser is successful is not only that they offer managed care, but integrated care. In a report from the Brookings Institute, they provide a simple graphic that explains the contractual relationship between members, physicians, and organizations; and how it aligns incentives across the organizations.
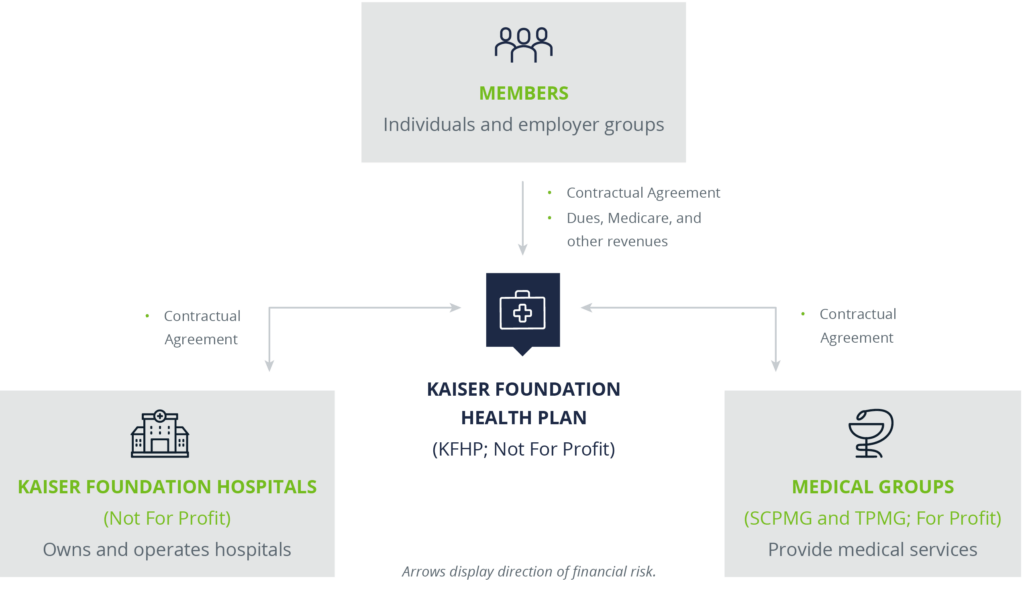
The financial incentive is to provide high quality, affordable care and manage population health rather than generating high volume of compensable services….The aligned structure and underlying contractual relationship between entities is the backbone that has led to the design of an efficient acute care delivery system that addresses a patient's needs across the continuum of care and maximizes population health.
—Brookings Institute
Four Key Characteristics Make Kaiser Different and Successful
Kaiser has been a model for healthcare for decades and their structure and investments show why they are a leader. In an interview with Robert Pearl, MD, CEO of The Permanente Medical Group, he stated the four key reasons that sets Kaiser apart, with an integrated healthcare model.
- Horizontal and Vertical Integration: All groups within the Kaiser system are integrated, from the health plan to departments, hospitals, and medical groups. This integrated approach creates a closed loop system for both outpatient and inpatient care.
- Prepaid Revenue: Over 90% of Kaiser's revenue is through prepaid premiums, aligning incentives between the organization and members. Without the worries of reimbursement, overhead may be lower, and Kaiser can use mobile technologies for payment.
- Comprehensive EHR: Kaiser invested in electronic EHR systems over 20 years ago and they are now available at every point of patient contact. This accessibility lowers costs by reducing unnecessary testing and physician communication barriers.
- Physician Leadership: Over 25% of physicians participate in Permanente Medical Group's Leadership Institute resulting in healthcare by health providers.
Can Traditional Insurers Compete?
Most of the innovations we see in healthcare are based on moves toward greater integration between providers, payers, and organizations to better the patient experience, reduce costs, and improve revenue streams.
Essentially, they are trying to replicate the Kaiser model that has been in effect for nearly 70 years. The healthcare system has major hurdles to overcome because it is made up of separate entities striving to integrate care and payment systems into a managed care environment.
We will continue to hear about enhanced integrated systems, cost-control efforts, predictive analysis, and the focus on the patient experience. These are all concepts that Kaiser has kept at the forefront and which insurers, hospitals, and providers strive to provide.
For more information about the Kaiser model, integrated models, and ways to maximize your Employee Benefits healthcare plans, contact your Woodruff Sawyer Account Team.
Author
Table of Contents